I’ve been recently thinking about stomach pain after hearing that a dear friend from the old country had been hospitalized with a peptic ulcer. This can be a very dangerous situation. Acute abdominal pain is a presenting complaint to be differentiated into referral or non-referral as quickly as possible. When in doubt, refer out, as they say. I have seen cases of perforating ulcers in my clinic that needed emergency surgery. It is not common, but it does happen from time to time. In cases where things are stable, Chinese medicine and acupuncture has a lot to offer.
So, in this edition of Clinical mulch, we will look at treating stomach pain from a few different sources: late imperial/early modern China, modern Chinese TCM, and contemporary Japanese acupuncture. First, here is an excerpt from Lèi Zhèng Zhì Cái [Differentiation and Classification of Patterns and Treatments] by Lín Pèiqín, published in 1839.
Stomach Pain Differentiations from Lèi Zhèng Zhì Cái
胃脘痛論治
胃脘當心下,主吸受飲食,若煩勞冷熱,致氣血痰食停瘀作痛,或肝氣犯胃,及腎寒厥逆,皆能致之。症與 心痛相似,但胃脘痛必見胃經本病,如脹滿、嘔逆、不食、便難、面浮、肢倦,與心痛專在包絡者自別。治法須分新久,初痛在經,久痛入絡,經主氣,絡主血也。初痛宜溫散以行氣,久痛則血絡亦痹,必辛通以和營,未可概以香燥例治也。
Stomach Duct Pain Discussion and Treatment
The stomach duct is just below the heart; it governs intake and receiving of food and drink. In case of vexation, overwork, cold or heat, the qì, blood, phlegm and food can lodge and stagnate causing pain; or liver qì can invade the stomach; cold from the kidney can reverse counterflow, all of these can be causes. This illness and heart pain resemble each other, but stomach pain will present with stomach channel root symptoms, such as distension and fullness, retching counterflow, inability to eat, difficult defecation, facial puffiness, and tired limbs; it is distinct compared to cases of heart pain located specifically in the pericardium. Treatment methods should separate recent [onset] from chronic. At first the pain is located in the channels and over time enters the network vessels; the channels govern qì, the networks govern blood. For early-stage pain use warm scattering to move qì. Later stage pain is caused by blood in the network vessels also becoming impeded. [In this case] one should use acrid and freeing [medicinals] to harmonize the provisioning yíng; one cannot generally use principles of aromatic drying to treat.
其因胃陽衰而脘痛者,食入不運,當辛甘理陽。香砂六君子湯加桂枝、良薑。
In cases caused by debilitation of stomach yang, with non-transportation of food, one should use acrid and sweet to regulate yáng. Xiāng Shā Liù Jūn Zǐ Tāng [Aucklandia and Amomum Six Gentlemen Decoction] plus Guì Zhī [Rm Cinnamomi] and Liáng Jiāng [Rz Alpiniae Officinarum].
因肝乘胃而脘痛者,氣衝脅脹,當辛酸制木。吳萸、白芍、青皮、木瓜、厚朴、延胡、金橘。
In cases caused by liver overwhelming the stomach with stomach duct pain, with qì surging and ribside distension, should use acrid and sour to restrain wood. Wú Yú [Rz Evodiae], Bái Sháo [Rx Paeoniae Alba], Qīng Pí [Pc Citri Reticulatae Viride], Mù Guā [Fr Chaenomelis], Hòu Pò [Cx Magnoliae Officinalis], Yán Hú [Rz Corydalis], Jīn Jú [Fr Fortunellae, kumquat].
因腎寒厥逆而脘痛者,吐沫嘔涎,當辛溫泄濁。吳茱萸湯。
In cases caused by reversal counterflow of kidney cold with stomach duct pain, vomiting froth and retching drool, should use acrid warming to discharge turbidity. Use Wú Zhū Yú Tāng [Evodia Decoction].
因煩勞傷氣而脘痛者,得食稍緩,當甘溫和中。小建中湯。
In cases caused by vexation and taxation damage to the qì with stomach duct pain, somewhat relieved by eating, should use sweet and warm to harmonize the center. Xiǎo Jiàn Zhōng Tāng [Minor Center Fortifying Decoction].
因客寒犯膈而猝痛者,嘔逆不食,當溫中散寒。大建中湯加白蔻仁。
In cases of lodged cold invading the diaphragm with sudden pain, retching counterflow and inability to eat, should use [the method of] warming the center to scatter cold. Dà Jiàn Zhōng Tāng [Major Center Fortifying Decoction] plus Bái Kòu Rén [Fr Amomi Kravanh].
積寒致痛,綿綿不絕,無增無減,當辛熱通陽。朮附湯加厚朴、草蔻。
Cold accumulation causing continuous unremitting pain, not increasing and not diminishing, should use acrid and warm to free yáng. Use Zhú Fù Tāng [Atractylodes and Aconite Decoction] plus Hòu Pò, Cǎo Kòu [Sm Alpiniae Katsumadai].
火鬱致痛,發則連日,脈必弦數,當苦辛泄熱。薑汁炒黃連、山梔瀉火為君,香附、川芎、陳皮、枳殼開鬱為臣,反佐炮姜,從治為使。
Fire depression causing pain and [heat] effusion for several days, the pulse will be wiry and rapid, one should use bitter and acrid to drain heat. Use Jiāng Zhī Chǎo Huáng Lián [Rz Coptidis fried in Succus Zingiberis, ginger juice] and Shān Zhī [Fr Gardeniae] to drain fire as sovereigns; Xiāng Fù [Rz Cyperi], Chuān Xiōng Rx Ligusticum Chuanxiong], Chén Pí [Pc Citri Reticulatae], Zhǐ Ké [Fr Aurantii] to open depression as ministers; and counteracting assistant Pào Jiāng [Rz Zingiberis Praeparatum] jointly treating as envoy.
痰積脘痛必嘔惡,清中湯加海石、南星、香附。
Phlegm accumulation stomach duct pain will have nausea and vomiting, use Qīng Zhōng Tāng [Center Clearing Decoction] plus Hǎi Shí [Pumice], Nán Xīng [Rz Arisaematis], and Xiāng Fù.
停飲脘痛必吞酸,胃苓湯、左金丸。
Lodged rheum stomach duct pain will have acid swallowing, use Wèi Líng Tāng [Stomach Calming Poria Five Decoction] and Zuǒ Jīn Wán [Left Metal Pill].
食滯脘痛必噯腐,香砂枳朮丸加半夏曲。
Food stagnation stomach duct pain will have putrid belching, use Xiāng Shā Zhǐ Zhú Wán [Aucklandia, Amomum, Aurantium, and Atractylodes Pill] plus Bàn Xià [Rz Pinelliae] and [Shén] Qū [Massa Fermentata Medicinalis].
氣鬱脘痛,必攻刺脹滿,沉香降氣散。
Qì depression stomach duct pain will have attacks of stabbing [pain], distension and fullness, use Chén Xiāng Jiàng Qì Sàn [Aquilaria Qì-Downbearing Powder].
傷力脘痛,必瘀血停留,鬱金、歸尾、桃仁、蘇木,或手拈散。
Injury with strong stomach duct pain will have blood stasis lodging, use Yù Jīn [Rx Curcumae], Guī Wěi [Rx Extremitas Angelicae Sinensis], Táo Rén [Sm Persicae], Sū Mù [Lignum Sappan], or Shǒu Niān Sàn [Instant Relief Powder].
怒氣脘痛,必呃逆胸痞,半夏瀉心湯。
Anger stomach duct pain will have hiccup and thoracic glomus, use Bàn Xià Xiè Xīn Tāng [Pinellia Heart-Draining Decoction].
蛔動脘痛,必有休止,安蛔丸。
Roundworm stomach duct pain will have resting and stopping [i.e. be intermittent], use [Lǐ Zhōng] Ān Huí Wán [Center-Rectifying Worm-Quieting Pill].
痛久不愈,必入血絡,歸鬚、桃仁、延胡、紫降香,或失笑散,效。
Pain which is chronic and unresolving will have entered the network vessels; using Guī Xū [Rx Tenuis Angelicae Sinensis], Táo Rén, Yán Hú, Zǐ Jiàng Xiāng [Lignum Dalbergiae], or Shī Xiào Sàn [Sudden Smile Powder], will be effective.
若痛而肢冷,脈微欲絕,桂心煎服甚效。
If there is pain with cold limbs, and a weak pulse on the verge of expiry, taking pan-fried Guì Xīn [Cx Cinnamomi Rasus] is effective.
Comment: The ingredients as given in the source text for the lesser-known formulas are:
· Zhú Fù Tāng is Bái Zhú, Fu Zĭ [Rx Aconiti Lateralis Praeparata], Gān Cǎo [Rx Glycyrrhizae], and Gán Jiāng [Rz Zingiberis].
· Qīng Zhōng Tāng is Huáng Lián, Shān Zhī, Chén Pí, Fú Líng, Bàn Xià, Gān Cǎo, Cǎo Kòu Rén [Sm Alpiniae Katsumadai], Sheng Jiāng [Rz Zingiberis Recens].
· Xiāng Shā Zhǐ Zhú Wán is Mù Xiāng [Rx Aucklandiae], Shā Rén [Fr Amomi], Zhǐ Ké, and Bái Zhú.
· Chén Xiāng Jiàng Qì Sàn is Chén Xiāng [Lignum Aquilariae], Shā Rén [Fr Amomi], Xiāng Fù, Zhì Gān Cǎo, and Sheng Jiāng.
· Shǒu Niān Sàn is Yán Hú Suǒ, Wǔ Líng Zhī [Excrementum Trogopteri], Cǎo Kòu Rén and Mò Yào [Myrrha].
· Lǐ Zhōng Ān Huí Tāng is Rén Shēn, Bái Zhú, Fú Líng, Gán Jiāng, Chuān Jiāo [Pc Zanthoxyli], Wū Méi [Fr Mume]
凡痛有虛實,按之痛止者為虛,按之痛反甚者為實。虛者,參朮散。實者,梔黃丸。痛甚者脈或伏,用藥不宜守補,參、耆、朮、地之屬。以痛則不通,通則不痛故也。
All pain has vacuity and repletion, cases in which pressure stops the pain are from vacuity, cases in which the pain increases with pressure are repletion. Vacuity cases, use Shēn Zhú Sàn [Ginseng and Atractylodes Powder]. Repletion cases, use Zhī Huáng Wán [Gardenia Yellow Powder]. In severe pain, the pulse may become hidden, in using medicinals it is inappropriate to keep supplementing with [Rén] Shēn, [Huáng] Qí [Rx Astragali], [Bái] Zhú, Dì Huáng [Rx Rehmanniae] types of substances. Because pain results from a lack of free passage, free passage will therefore result in a lack of pain.
Comment:
· Shēn Zhú Sàn is Rén Shēn, Bái Zhú, and Gān Cǎo, i.e., Sì Jūn Zǐ Tāng [Four Gentlemen Decoction] without Fú Líng,
· Zhī Huáng Wán may be a misprint. In the formula list that follows, Lin lists for repletion pain a different formula, Zhī Yú Wán [Gardenia and Evodia Pills, 梔萸丸] which is given in the source text as Shān Zhī and Wú Zhū Yú with a possible addition of Xiang Fu. There is always the possibility that Zhī Huáng Wán is a combination of Shān Zhī with Huáng Lián, which would not be inappropriate in this case. Many cases of stomach ulcers are caused by infection of H. Pylori, and the broad spectrum of antibiotic action of this combination would likely be effective in treating those particular circumstances.
胃脘痛脈候
弦為痛,澀為痛。胃脈微滑為痰飲,滑實為宿食。沉緊為冷積,沉澀為氣滯。數大為火,芤弦為血,忽大忽小為蟲。沉小者生,實大浮長者死。
Stomach Duct Pain Pulse Signs
Wiry because of pain, rough because of pain. Stomach pulse is weak and slippery because of phlegm-rheum, [or] slippery and replete because of lodged food. Sinking and tight because of cold accumulation, [or] sinking and rough because of qì stagnation. Rapid and large because of fire, [or] hollow and wiry because of bleeding, or suddenly large then suddenly small because of worms. Cases where it is sinking and small will live, cases where it is replete, large, floating and long will die.
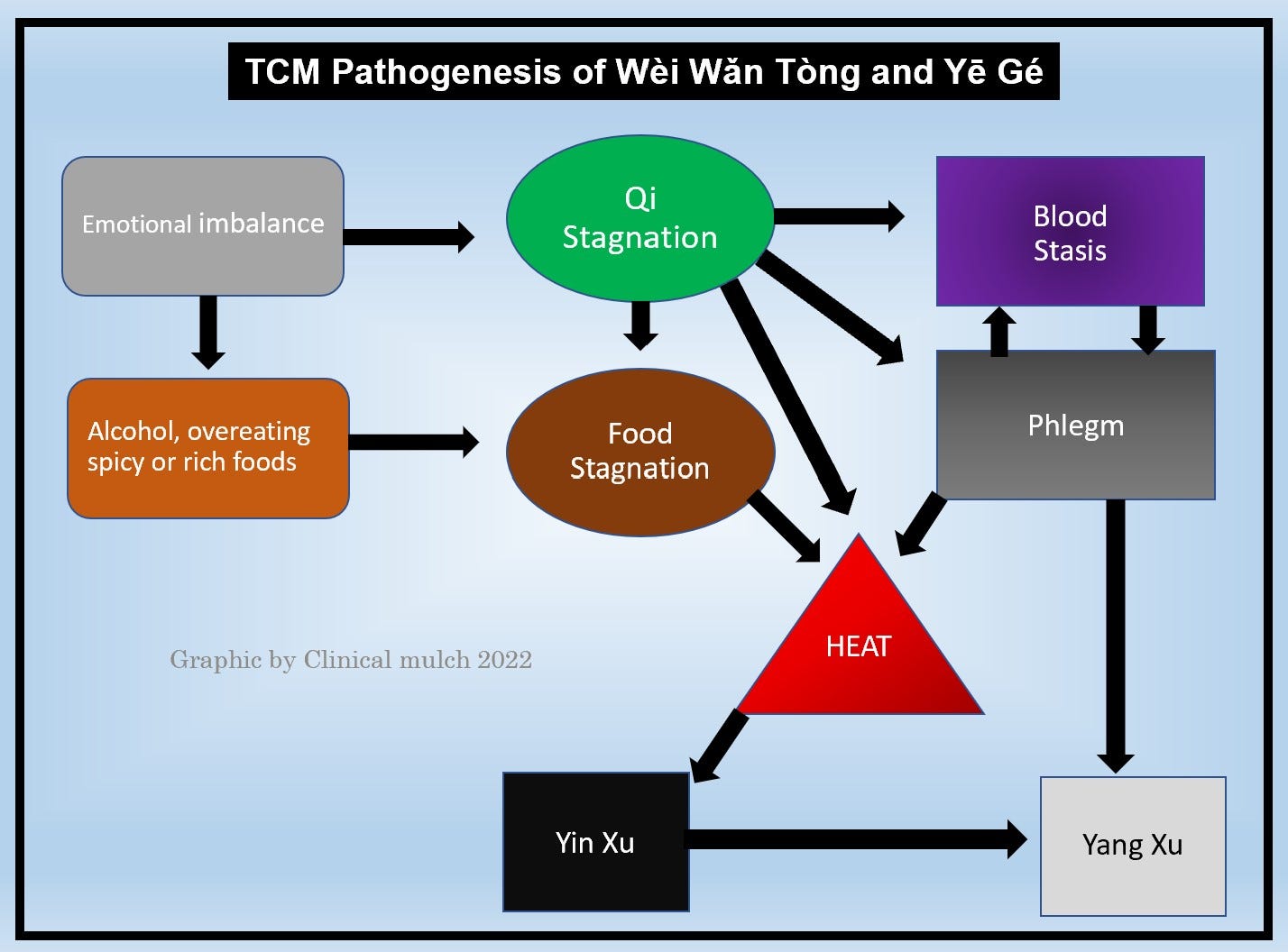
Modern TCM Pathogenesis Chart
Here is a chart I put together a couple of years ago for my students at East West College. It is meant to show the formation of Yē Gé (dysphagia-occlusion, i.e. reflux) but is basically the same as for stomach duct pain, to which it is related. The text used for the course was Wu & Fischer (1997). There are minor differences from Lèi Zhèng Zhì Cái, which came a hundred-and-some years earlier, most notably the development of yīn vacuity of the stomach and kidneys. This is in my experience an important addition, for which formulas containing Mài Mén Dōng [Tuber Ophiopogonis], such as Yī Guàn Jiān (Linking Decoction), can be helpful.
Acupuncture Perspectives on Stomach Pain
Now we’ll look at some acupuncture approaches for stomach pain. First here is one from the Zhēn Jiǔ Féng Yuán (Encountering the Origins of Acumoxa, 1815) a Qīng era text by Lǐ Xuéchuān:
胃脘痛 內關 膈俞 胃俞 商丘
Stomach Duct Pain: Nèi Guān [PC6], Gé Shù [UB17], Wèi Shù [UB21], Shāng Qiū [SP5]
And then one from Zhēn Jiǔ Dà Chéng (Great Compendium of Acupuncture and Moxibustion, 1601), a famous Míng era text by Yáng Jìzhōu:
胃脘痛:太淵 魚際 三里 兩乳下(各一寸,各三十壯); 膈俞 胃俞 腎俞(隨年壯)
Stomach Duct Pain: Tài Yuān [LU9], Yú Jì [LU10], Sān Lǐ [ST36], liǎng rǔ xià [below each breast] (each 1 cùn, each 30 rounds of moxa); Gé Shù [UB17] Wèi Shù [UB21], Shèn Shù [UB23], (follow the patient’s age for number of rounds of moxa).
For me, the point combination in the Féng Yuán has a familiar ring to it: it is a five-phase spleen pattern, with a combination of spleen and pericardium channels, same as I use every day in clinic. PC6 is well-known for treating stomach problems as well as coursing qì in general. SP5 is the metal point, which is often thought of as the “sedation” point, though I associate the metal-ness of it with the acrid taste that scatters and moves. UB17 is the huì xué/meeting point for the blood, and UB21 is the back point for the stomach. This combination looks to treat mainly stagnation of qì, blood and fluids affecting the stomach.
The point combination in the Dà Chéng takes a different approach. It treats the lung channel – not an obvious connection but one that brings to mind some interesting ideas. First, the lung channel begins in the middle burner. I frequently say to my students that Zhōng Wǎn [CV12] can be thought of as the first point on the lung channel; it is also the alarm point of the stomach. ST36 is of course a major point for the stomach. Treating below the breasts is treating along the stomach channel, as well as addressing the diaphragm area, which we will come back to in a moment. The back points are the same as in the later Féng Yuán, with an interesting difference: the back point for the kidney, UB23, is treated. In terms of the yīn organs addressed here, kidney and lung, this makes a kinda-sorta 5-phase kidney pattern. The moxa count depends on the patient’s age; so if the patient is 46, then use 46 rounds of moxibustion.
Speaking of 5-phases, let’s look at an approach from Japanese 5-phase keiraku chiryo (meridian therapy), my home turf in terms of acupuncture style.
Shudo Denmei’s Treatment of Stomach Pain
I’ve had the great fortune to have attended Shudo Denmei’s annual seminars for several years running, back around the turn of the century. Among the notes I have are some of the treatments he would use for stomach pain. Much of the material he taught then made it into his 2003 book, Finding Effective Acupuncture Points.
Shudo sensei would typically treat stomach problems as a spleen pattern (using SP3 as the main supplementing point), or a kidney pattern (using KD7). Interestingly, this differentiation is echoed by the treatments we saw in the Féng Yuán (spleen pattern) and Dà Chéng (kidney pattern) earlier. In terms of five-phase dynamics, one could see the stomach pain as arising from a yīn-yáng imbalance within the earth phase (spleen root pattern) or arising from a ten-stem imbalance between water yīn and earth yáng (kidney root pattern)
Shudo sensei also talked about abdominal signs he will look for, especially along the stomach channel. If ST24, for example, is reactive – that is to say tender on pressing or pinching up the skin over the point – Shudo will suspect a duodenal ulcer. Tenderness at the ST19-21 area on the left can denote stomach problems and on the right can indicate problems with the gallbladder.
I typically will extend this to the back, especially in the area of UB17-UB19, which is to say the spinal level of the diaphragm, liver, gallbladder, as well as the stomach duct. There are often rubbery indurated areas to which I will apply needles and/or direct moxa. I see this area is often reactive whether stomach pain, acid reflux, and so forth is a primary complaint or one of a long list of problems.
Onodera point
Shudo (2003) also writes about the Onodera point, which is a reactive zone discovered by a Japanese physician that correlates with peptic ulcer. It is approximately 5 cm (about 2 inches) below the iliac crest, on the upper gluteals. Though Onodera would palpate with the patient lying on their side, Shudo maintains that it is easier to find with the patient lying prone (face down). Begin by pressing along an imaginary line 5 cm below the iliac crest, starting at the anterior end and finishing below the posterior iliac spine. The line is divided into thirds, from front to back: the first third represents the esophagus, the middle third represents the stomach duct (upper stomach) and the last third represents the lower stomach and duodenum. A positive finding (usually a hardened area which is tender on pressing) on the left suggests a gastric ulcer and a positive finding on the right suggests a duodenal ulcer; the latter is especially so if it is combined with a positive finding at ST24 (Shudo, 2003, pg 228). A longer needle and deeper insertion is usually necessary to treat the point.
Conclusion
As we have seen, there are many different approaches one can take to treating stomach pain; we have looked at just a few of the possibilities. Non-emergency cases of stomach pain can find help with symptoms, tissue healing, and prevention of relapse with acupuncture and Chinese medicine.
That’s all for now; as always, thanks for reading.
Note: this publication is for information purposes only and is not intended as medical advice. Please seek the opinion of a health care professional for any specific medical issues you may have.
References
Lǐ, X. (1815). Zhēn jiǔ féng yuán. https://jicheng.tw/tcm/book/%E9%87%9D%E7%81%B8%E9%80%A2%E6%BA%90/index.html. Retrieved December 16, 2022.
Lín , P. (1839). Lèi zhèng zhì cái. https://jicheng.tw/tcm/book/%E9%A1%9E%E8%AD%89%E6%B2%BB%E8%A3%81/index.html. Retrieved January 14, 2024.
Shudo, D. (2003). Finding effective acupuncture points (S. Brown, Trans.). Eastland Press.
Wu, Y., & Fischer, W. (1997). Practical therapeutics of traditional Chinese medicine. Paradigm Publications.
Yáng, J. (1601). Zhēn jiǔ dà chéng. https://jicheng.tw/tcm/book/%E9%87%9D%E7%81%B8%E5%A4%A7%E6%88%90/index.html. Retrieved December 26, 2023.