Last month I wrote about plastic accumulation in the brain, and possible measures to aid the body in clearing the pathogenic burden. The research for that article opened up several interesting avenues of exploration, one of which I present today.
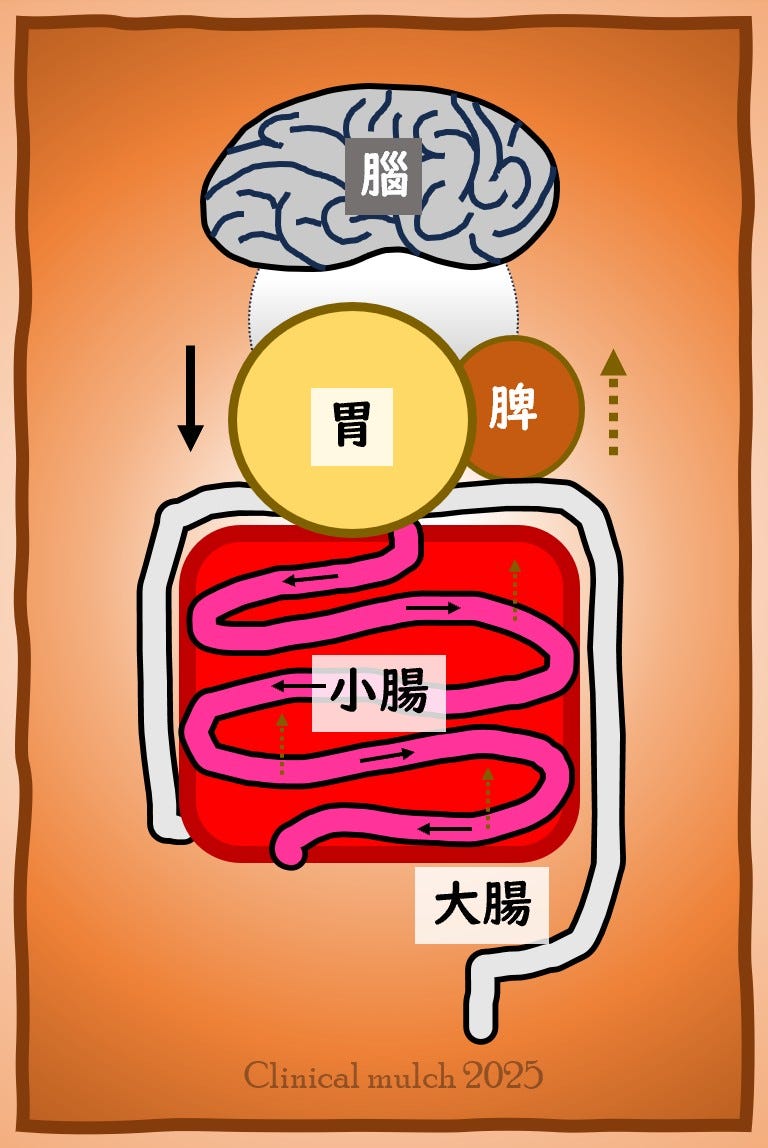
A hot topic that has emerged in recent years is the “brain-gut axis [脑 肠轴 nǎocháng zhóu]” and its treatment in Chinese medicine, sometimes called the “brain-gut co-regulation treatment method [脑肠同调治法 Nǎocháng tóngtiáo zhìfǎ]”. I will focus specifically on acupuncture treatment of the brain-gut axis in this article.
The Brain-Gut Axis
The brain-gut axis is a bi-directional feedback system between the central nervous system and the gastrointestinal tract. It is a neuro-endocrine-immune complex consisting of many overlapping components, including the central nervous system (CNS), autonomic nervous system (ANS), enteric nervous system (ENS) and the hypothalamus-pituitary-adrenal axis (HPA) (Guo et al., 2024). Intestinal flora (microorganisms such as bacteria, fungi, etc.) help support brain function through regulating brain-gut peptides, which are short chains of amino acids found in both the brain and intestines; they influence such things as appetite and digestion, as well as mood – one example is 5-hydroxytryptamine [a.k.a serotonin] which is synthesized in the gut and present in both the brain and digestive tract (Bu et al., 2024).
Overgrowth or lack of diversity of intestinal flora can lead to pathogenic states: certain species of Bacteroidetes and Enterobacteriaceae, for example, can produce large amounts of inflammatory metabolites (LPS) which can leak into the body through the damaged intestinal barrier, aggravating the body’s inflammatory response that can affect the permeability of the blood-brain barrier (BBB) and cause damage to the nervous system. Patients with CNS diseases (Parkinson’s Disease, Multiple Sclerosis, stroke) have been shown to have a decrease in gut microbiome diversity and overgrowth of potentially pathogenic strains of Bacteroidetes, Enterobacteriaceae, Oscillospiraceae, and Clostridiaceae (Jiang et al., 2024).
TCM and the Brain-Gut Axis
TCM has no brain-gut axis per se, but there is a rich history of writings connecting the organs and emotions. The brain-gut inter-relationship is often explained indirectly by means of theories such as heart-spleen and liver-spleen inter-relationships (Wang et al., 2025). However there are some writings which reference the stomach and intestines [which are often referred to as a coherent unit, 胃肠, wèicháng] and their influence on the brain and emotions. For example, Líng Shū 30 [灵枢·决气, “Understanding the qì”] links the stomach and small intestine, which governs fluid, to the brain:
谷入气满,淖泽注于骨,骨属屈伸,泄泽,补益脑髓,皮肤润泽,是谓液.
When grains enter [the stomach], the qì is full, and the swampy moisture pours into the bones so the bone joints can bend and stretch. Then the moisture is discharged to supplement and boost the brain marrow and lubricate the skin. This is called fluid.
The large intestine, for its part, governs conveyance of the dregs, and the dregs descend while clear qì ascends to moisten and nourish the brain orifices (Wang et al., 2025).
Let’s take a look at some of the literature around the brain-gut axis, its associated pathologies, and some of the treatment strategies currently being used to treat it.
Stroke and the Brain-Gut Axis
Jiang et al. (2024) looked at the brain-gut co-regulation method and its effect on sequelae of ischemic stroke. 82 subjects with hemiplegia from ischemic stroke were enrolled in the study. Measurement included the Fugl-Meyer assessment scale, which measures activities of daily living including motor and sensory function, balance, and joint range and pain. Both control and experimental groups were given standard rehabilitative care and any particular treatments for blood pressure, blood glucose and lipids, etc.
Both groups received acupuncture. The control group received a standard post-stroke protocol consisting of GV20, Yìntáng, and bilateral GB20 and ST36; also treated were LI4, LI11, LI15, TB5, ST32, SP6 and LR3, all on the affected side.
The experimental group was given treatment with the brain-gut co-regulation method. The points chosen were the scalp anterior parietal-temporal line (MS-6, the line from the anterior Sìshéncōng point to GB6) on the affected side, plus CV12, and CV4, along with bilateral ST25, ST36, ST37, and ST39.
The point selection in this study was quite straightforward:
MS-6: Brain’s motor and sensory area
CV12: Stomach mu point
ST25: Large intestine mu
CV4: Small intestine mu point
ST36-37-39: lower he sea points for Stomach, Large intestine, Small intestine respectively
After obtaining qì, the needles were retained for 30 minutes. Treatment was once daily, five days a week, for 4 weeks. One physician performed all treatments.
Evaluation scores were comparable between the groups before the study, and after it was completed the experimental group was significantly improved over the control group.
In addition to the motor, sensory, balance, and pain improvements, the study measured gut flora and noted improvements with acupuncture, again with significant improvement of the experimental group over the control. The experimental group in this study showed a decrease in both pathogenic strains of gut bacteria and associated inflammatory markers such as TNF-α, IL-1β, and IL-6, as well as increased beneficial strains of Lachnospiraceae, Ruminococcaceae, and Bifidobacteriaceae. This suggests that acupuncture and particularly point prescriptions aimed at the brain-gut axis can help improve the severity of the disease state by regulating and improving the balance of gut flora, inhibiting the proliferation of inflammatory agents and strengthening the integrity of the intestinal barrier.
故神者,水谷之精气也.
Thus the spirit is the essence qì of water and grain.
Líng Shū (32), “When Healthy People Stop Eating [平人绝谷]”
Depression and the Brain-Gut Axis
As mentioned earlier, the brain-gut peptides such as serotonin, present in both the brain and intestines, have a direct influence on mood. Treatment of depression, according to Bu et al. (2024), needs to take into account the regulation of gastrointestinal function as well as neuropsychiatric function. Patients with depression often have gastrointestinal symptoms, such as alternating diarrhea and constipation, bowel sounds, and increased flatulence.
Bu et al. (2024) presented a paper on the application of the “Free depression and awaken the brain” acupuncture treatment method [达郁醒脑针刺治疗, Dáyù xǐngnǎo zhēncì zhìliáo]. The method is based on several elements:
Abdominal acupuncture to rectify the spleen, regulate the qì, and free the bowels. Abdominal acupuncture points lie mostly on the stomach, kidney, and rèn channels. The stomach channel enters the brain, the kidney has a strong relation to the brain, and the rèn mài both shares an origin with the dū mài and intersects with the foot yángmíng stomach channel at ST1, and so is linked to the brain as well. The abdominal portion of the method is oriented around CV8, the center of the navel. CV8 is not just important embryonically, say the authors; it distributes qì and runs the qì mechanism. Thus CV8 has a profound effect on regulating the transportation and allocation of qì and blood through the whole body. The main abdominal points used in the method are CV12, CV10, CV6, CV4; plus bilateral ST23, ST24, ST26, SP15. Shallow needling is done to reach the superficial fascia and retained for 30 minutes. ST24 and ST26 are the “abdominal 4 gates”, while SP15 is horizontal axis to CV8. ST23 is added because of its traditional psychoemotional indications.
Head acupuncture to open the du mai, regulate the spirit, awaken the brain, and resolve depression. Points selected are GV20, GV24, Sìshéncōng and Yìntáng. The points all lie along the trajectory of the dū mài, which enters the brain. Sìshéncōng is punctured so the needles all reach toward GV20.
Four gates to promote movement through the brain-gut pathway. As the source points for the large intestine and liver, representing the dynamic phases of metal and wood, LI4 and LR3 have a powerful synergy in regulating the qì of the whole body, connecting the upper and lower to promote the proper ascending and descending of the qì mechanism. The point combination is used to both free depression and ensure proper qì flow between gut and brain.
四關者,六臟有十二原,出於四關,太衝、合谷是也。
The four gates are the 12 origins (i.e. source points) of the six viscera; they emerge from the four gates, which are LR3 and LI4.
針灸大成 , Zhēnjiǔ Dàchéng (1601)
Autism Spectrum Disorder and the Brain-Gut Axis
Wang et al. (2025) reported on a study involving acupuncture based on treating the brain-gut axis in combination with sensory integration training in children diagnosed with Autism Spectrum Disorder (ASD). 70-80% of children with ASD have some sort of GI disturbance such as diarrhea, bloating, or constipation. ASD can be classified under TCM category of juvenile clouding [童昏 tónghūn], or delayed speech [语迟 yǔchí]. The disease cause and mechanism is associated with pre-heaven spleen and kidney insufficiency [脾肾不足], brain deprived of nourishment [脑失所养], obstructed heart orifices [心窍不通], and brain network stasis block [脑络瘀阻]. Heart and spleen dual vacuity is commonly seen, and one should free the channels and quicken the networks [通经活络], strengthen the transporting function of the spleen and stomach [健运脾胃], arouse the brain and open the orifices [醒脑开窍] as treatment principles.
The study involved 90 children ages 2-7 with diagnosis of ASD and TCM diagnosis of spleen vacuity. The control group received sensory integration training, and the experimental group received both the sensory integration training and acupuncture. The point prescription was as follows:
Five needles on the forehead:
GV24: settles, tranquilizse and calms spirit, sharpens the wits and engenders wisdom [镇静安神、益智生慧]
ST8 and GB15: anterior gyrus of the frontal lobe – higher level language area, emotions, memory
Sìshéncōng: frees the brain and awakens the spirit, stengthens the brain and boosts marrow [通脑醒神、健脑益髓]
Body acupuncture
GV7* and ST25 strengthen spleen and harmonize stomach [健脾和胃]
UB15 and UB20 strengthen spleen and calm the spirit [健脾宁神]
ST36 regulates qì mechanism of the stomach and intestines [调理胃肠之气机]
LI4 and LR3 regulate and harmonize qì and blood, rectify qì and free the bowels [调和气血、理气通腑]
*The point cited was 中枢 Zhōngshū which is the name for GV7. However, I wonder if the point treated was not actually CV12 中脘 Zhōngwǎn given the pairing and indications stated above.
The primary outcome measure was the Autism Behavior Checklist (ABC) score, and further rating scales for behavior, language, etc; gastrointestinal symptoms were also used. In addition, the abundance of intestinal flora was measured. All scores improved with treatment in both groups, with the experimental group showing greater improvement than the control group. In the measurement of intestinal flora, the Escherichia coli and Enterococcus count was decreased in both groups, with the experimental group lower than the control, and the relative abundance of Bifidobacterium and Lactobacillus had increased in both groups, again with the experimental group being greater.
The researchers believe that acupuncture works through the brain-gut axis to regulate gastrointestinal motility and intestinal flora, reduce harmful gut microbes, and increase the numbers of beneficial flora. Thus it is postulated that by improving the gut environment, acupuncture can help promote neurodevelopment through the bidirectional communication mechanism of the brain-gut axis.
Parkinson’s Disease and the Brain-Gut Axis
Fan et al. (2024) published an article on using acupuncture in treating Parkinson’s Disease (PD), based on the concept of the brain-gut axis. While there were no specific clinical or research protocols, the article was nevertheless quite interesting.
Researchers have postulated an “intestinal origin theory” of PD and a growing body of evidence suggests that the brain-gut axis has a crucial part in the development of the disease. Acupuncture has been shown to improve both motor and non-motor aspects of PD, and this paper was aimed at examining possible mechanisms of action involving the brain-gut axis.
Evidence shows that the intestinal microbial environment changes with the progression of PD, and such changes may correlate with the severity of the disease process. A decrease in Faecalibacterium, for example, is associated with a decrease in short-chain fatty acids (SCFA) which leads to intestinal inflammation and an increase in permeability of the intestinal barrier, as well as abnormal aggregations of α-Syn (a pre-synaptic neuronal protein that, if it becomes misfolded, acts similar to a prion, causing nervous system degeneration). Accumulation of α-Syn in the intestines can spread to the CNS, triggering neuroinflammation, damaging dopamine neurons, and accumulating in Lewy bodies in the brain.
Another factor is the involvement of the vagus nerve, which is postulated as a high-speed route for pathogenic accumulations of α-Syn to travel out of the enteric nervous system (ENS) to the brain. Non-invasive vagus nerve stimulation has been tried on PD patients and found to improve such factors as gait, showing that vagal intervention can be beneficial in treating PD patients.
Overactivation of the HPA axis can induce oxidative stress and disrupt the normal balance of intestinal flora through its release of glucocorticoids. On the other hand, research has shown that introduction of beneficial strains of bacteria into the gut can restore depressed HPA activity and alleviate stress-induced anxious behaviors. PD patients frequently have glucocorticoid imbalance, which can ultimately lead to persistent brain inflammation and oxidative stress.
Acupuncture can regulate and improve diversity of the intestinal flora, inhibit the expression of pro-inflammatory factors such as IL-6 and TNF- α, regulate the vagus nerve to promote to proper digestive motility, foster the release of catecholamines (such as dopamine), inhibit overactivation of the HPA axis and reduce levels of corticotropin-releasing hormone (CRH) and adrenocorticotropic hormone (ACTH), and regulate levels brain-gut peptides.
In terms of TCM, the authors state that PD belongs to wind syndromes due to vacuity of liver, spleen and kidney [肝、脾与肾三脏虚衰], and lack of nourishment to the sea of marrow [髓海失养], with wind, fire, phlegm and blood stasis types of evils stagnating in the brain networks [风、火、痰与瘀等邪实阻滞脑络].
Conclusion
With regard to treating various neurodegenerative diseases, as well as digestive diseases which are triggered by emotional stress, the brain-gut axis has become a focus of interest in acupuncture and Chinese medicine. While there is no explicit link between the brain and the intestines in classical Chinese texts, there are ways to approach the connection in order to formulate a theoretical foundation for treatment.
Research has shown that acupuncture can activate physiological mechanisms to change the body’s internal environment, including the gut microbiome. Jiang et al. (2024) found that a point prescription specifically geared toward addressing the brain-gut axis was more effective in increasing microbiome diversity, increasing beneficial gut flora and decreasing potential disease-causing microbes than one which was aimed at treating the presenting complaint, even improving the symptoms to a greater degree than the control group points.
In terms of point formula composition, the three examples given above had a similar structure. Points on the head - whether points on the dū mài or extra points such as GV20, GV24, Sìshéncōng, and so forth, or scalp acupuncture lines such as MS-6 – are combined with points on the abdomen and perhaps the back as well. Points related to the stomach and intestines, especially on the foot yángmíng stomach channel, are well suited to this method. Powerful channel points such as the Four Gates, LI4 and LR3, may be added as well.
While the integration of the brain-gut axis into TCM theory is still early in its development, the prospect of future research into changes in the body’s microbiome with acupuncture seems quite promising, and likely to lead to new insights into acupuncture’s physiological mechanisms and its ability to treat a wide range of conditions.
That’s all for now, thanks for reading.
Note: this publication is for information purposes only and is not intended as medical advice. Please seek the opinion of a health care professional for any specific medical issues you may have.
References
Bu, R., Teng, J., & Qí, X. (2024). Treating depression by the Dayu Xingnao acupuncture based on the brain gut axis theory. Clinical Journal of Chinese Medicine, 16(14),105-109. doi: 10.3969/j.issn.1674-7860.2024.14.019
Fan S., Sun, Y., Yan, L., Qian, Y., & Yu, T. (2024). Exploring mechanism of acupuncture and moxibustion in treatment of PD based on brain-gut axis theory. Journal of Clinical Acupuncture, 40(12), 90-95. DOI:10.19917/j.cnki.1005-0779.024240
Guo, X., Gao, S., Jiang, F., & Wang, X. (2024). Exploration of Hewei Anshen acupuncture in treatment of generalized anxiety disorder based on brain-gut axis. Journal of Clinical Acupuncture, 40(10), 101-105. DOI:10.19917/j.cnki.1005-0779.024203
Jiang, Z. , Liu, L. , Zhang, L. , Li, L. , Ding, B. , Hu, L. , & Wu, Z. (2024). Effects of "brain-gut coherence" method of acupuncture on motor function and intestinal microflora in the patients with cerebral ischemic stroke. Chinese Acupuncture & Moxibustion, 44(07), 740-748. DOI: 10.13703/j.0255-2930.20231109-k0009
Wang, N., Wang, G., Chen, D. (2025). Efficacy of acupuncture based on "gut-brain axis" combined with sensory integration training on autism spectrum disorder and its effect on gastrointestinal symptoms. Chinese Acupuncture & Moxibustion, 45(1), 36-40, 60. DOI:10.13703/j.0255-2930.20240318-k0001
Wang, R., Zeng, H., & Liu, B. (2025). Discussion on the multi-dimensional pathways of acupuncture treatment for encephalopathy. Journal of Nanjing University of Traditional Chinese Medicine, 41(2), 189-194. DOI: 10.14148/j.issn.1672-0482.2025.0189